Supracondylar fractures of the humerus are one of the most common fractures in children and occur at the junction of the humeral shaft and the humeral condyle.
Clinical Manifestations
Supracondylar fractures of the humerus are mostly children, and local pain, swelling, tenderness, and dysfunction may occur after injury. Undisplaced fractures lack obvious signs, and elbow exudation may be the only clinical sign. The joint capsule below the elbow muscle is the most superficial, where the soft joint capsule, also known as the softspot, can be palpated during joint exudation. The point of flexibility is usually anterior to the line connecting the center of the radial head to the tip of the olecranon.
In the case of a supracondylar type III fracture, there are two angulated deformities of the elbow, giving it an S-shaped appearance. There is usually subcutaneous bruising in front of the distal upper arm, and if the fracture is completely displaced, the distal end of the fracture penetrates the brachialis muscle, and the subcutaneous bleeding is more serious. As a result, a pucker sign appears in front of the elbow, usually indicating a bony protrusion proximal to the fracture penetrating the dermis. If it is accompanied by radial nerve injury, the dorsal extension of the thumb may be limited; median nerve injury may cause the thumb and index finger to be unable to actively flex; ulnar nerve injury may result in limited division of fingers and interdigitation.
Diagnosis
(1) Diagnosis Basis
①Have a history of trauma; ②Clinical symptoms and signs: local pain, swelling, tenderness and dysfunction; ③X-ray shows the supracondylar fracture line and displaced fracture fragments of the humerus.
(2) Differential Diagnosis
Attention should be paid to the identification of elbow dislocation, but the identification of extensional supracondylar fractures from elbow dislocation is difficult. In the supracondylar fracture of the humerus, the epicondyle of the humerus maintains a normal anatomical relationship with the olecranon. However, in elbow dislocation, because the olecranon is located behind the epicondyle of the humerus, it is more prominent. Compared with supracondylar fractures, the prominence of the forearm in elbow dislocation is more distal. The presence or absence of bony fricatives also plays a role in identifying supracondylar fractures of the humerus from dislocation of the elbow joint, and it is sometimes difficult to elicit bony fricatives. Because of the severe swelling and pain, manipulations that induce bony fricatives often cause the child to cry. Because of the risk of neurovascular damage. Therefore, manipulations that induce bone fricatives should be avoided. X-ray examination can help identify.
Type
The standard classification of supracondylar humeral fractures is to divide them into extension and flexion. The flexion type is rare, and the lateral X-ray shows that the distal end of the fracture is located in front of the humeral shaft. The straight type is common, and Gartland divides it into type I to III (Table 1).
|
Type |
Clinical Manifestations |
|
ⅠA type |
Fractures without displacement, inversion or valgus |
|
ⅠB type |
Mild displacement, medial cortical fluting, anterior humeral border line through humeral head |
|
ⅡA type |
Hyperextension, posterior cortical integrity, humeral head behind the anterior humeral border line, no rotation |
|
ⅡB type |
Longitudinal or rotational displacement with partial contact at either end of the fracture |
|
ⅢA type |
Complete posterior displacement with no cortical contact, mostly distal to medial posterior displacement |
|
ⅢB type |
Obvious displacement, soft tissue embedded in the fracture end, significant overlap or rotational displacement of the fracture end |
Table 1 Gartland classification of supracondylar humerus fractures
Treat
Before optimal treatment, the elbow joint should be temporarily fixed in a position of 20° to 30° flexion, which is not only comfortable for the patient, but also minimizes the tension of neurovascular structures.
(1) Type I humeral supracondylar fractures: only need a plaster cast or cast cast for external fixation, usually when the elbow is flexed 90° and the forearm is rotated in a neutral position, a long arm cast is used for external fixation for 3 to 4 weeks.
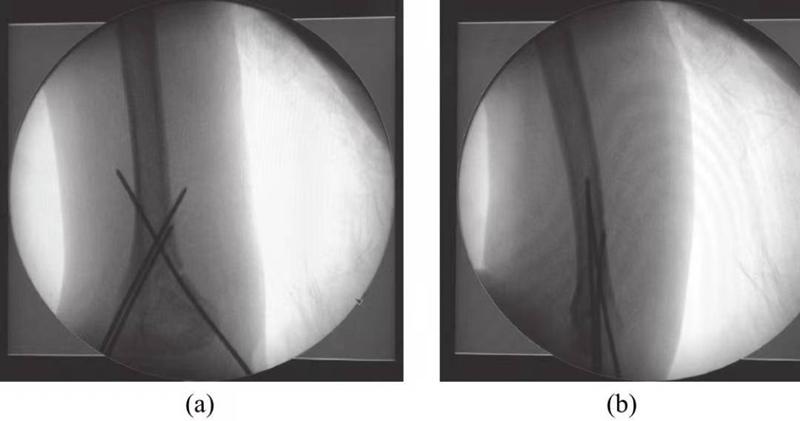
(2) Type II humeral supracondylar fractures: Manual reduction and correction of elbow hyperextension and angulation are the key issues in the treatment of this type of fractures. °) The fixation maintains the position after reduction, but increases the risk of neurovascular injury of the affected limb and the risk of acute fascial compartment syndrome. Therefore, percutaneous Kirschner wire fixation is best after closed reduction of the fracture (Fig. 1), and then External fixation with a plaster cast in a safe position (elbow flexion 60°).
Figure 1 Image of percutaneous Kirschner wire fixation
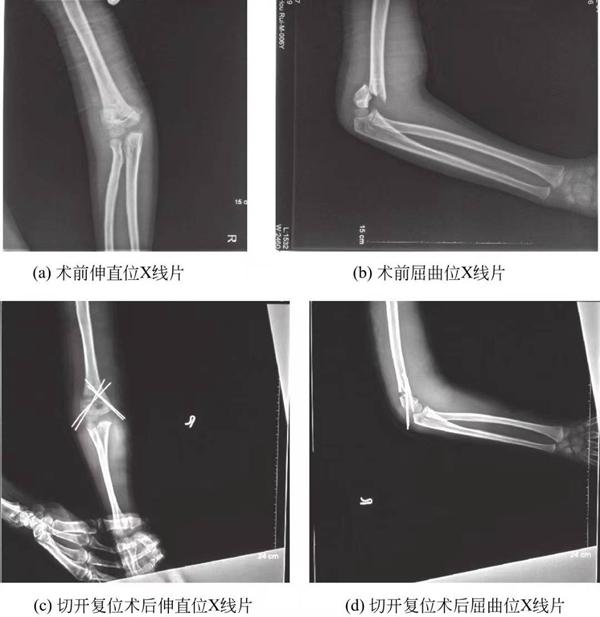
(3) Type III supracondylar humerus fractures: All type III supracondylar humerus fractures are reduced by percutaneous Kirschner wire fixation, which is currently the standard treatment for type III supracondylar fractures. Closed reduction and percutaneous Kirschner wire fixation are usually possible, but open reduction is required if the soft tissue embedding cannot be anatomically reduced or if there is brachial artery injury (Figure 2).
Figure 5-3 Preoperative and postoperative X-ray films of supracondylar humerus fractures
There are four surgical approaches for open reduction of supracondylar fractures of the humerus: (1) lateral elbow approach (including anterolateral approach); (2) medial elbow approach; (3) combined medial and lateral elbow approach; and (4) posterior elbow approach.
Both the lateral elbow approach and the medial approach have the advantages of less damaged tissue and simple anatomical structure. The medial incision is safer than the lateral incision and can prevent ulnar nerve damage. The disadvantage is that neither of them can directly see the fracture of the contralateral side of the incision, and can only be reduced and fixed by hand feeling, which requires a higher surgical technique for the operator. The posterior elbow approach has been controversial due to the destruction of the integrity of the triceps muscle and the greater damage. The combined approach of the medial and lateral elbows can make up for the disadvantage of not being able to directly see the contralateral bone surface of the incision. It has the advantages of the medial and lateral elbow incisions, which is conducive to fracture reduction and fixation, and can reduce the length of the lateral incision. It is beneficial to the relief and subsidence of tissue swelling; but its disadvantage is that it increases the surgical incision; Also higher than the posterior approach.
Complication
Complications of supracondylar humeral fractures include: (1) neurovascular injury; (2) acute septal syndrome; (3) elbow stiffness; (4) myositis ossificans; (5) avascular necrosis; (6) cubitus varus deformity; (7) cubitus valgus deformity.
Summarize
Supracondylar fractures of the humerus are among the most common fractures in children. In recent years, poor reduction of supracondylar fractures of the humerus has aroused people's attention. In the past, cubitus varus or cubitus valgus was considered to be caused by the arrest of growth of the distal humeral epiphyseal plate, rather than poor reduction. Most of the strong evidence now supports that poor fracture reduction is an important factor in cubitus varus deformity. Therefore, reduction of supracondylar humerus fractures, correction of ulnar offset, horizontal rotation and restoration of distal humerus height are the keys.
There are many treatment methods for supracondylar fractures of the humerus, such as manual reduction + external fixation with plaster cast, olecranon traction , external fixation with splint , open reduction and internal fixation , and closed reduction and internal fixation. In the past, manipulative reduction and plaster external fixation were the main treatments, of which cubitus varus was reported as high as 50% in China. At present, for type II and type III supracondylar fractures, percutaneous needle fixation after reduction of the fracture has become a generally accepted method. It has the advantages of not destroying blood supply and fast bone healing.
There are also different opinions on the method and optimal number of Kirschner wire fixation after closed reduction of fractures. The editor's experience is that the Kirschner wires should be bifurcated with each other during fixation. The farther apart the fracture plane is, the more stable it is. The Kirschner wires should not cross at the fracture plane, otherwise the rotation will not be controlled and the fixation will be unstable. Care should be taken to avoid damage to the ulnar nerve when using medial Kirschner wire fixation. Do not thread the needle in the flexed position of the elbow, slightly straighten the elbow to allow the ulnar nerve to move back, touch the ulnar nerve with the thumb and push it back and safely thread the K-wire. The application of crossed Kirschner wire internal fixation has potential advantages in postoperative functional recovery, fracture healing rate, and excellent rate of fracture healing, which is beneficial to early postoperative recovery.
Post time: Nov-02-2022